
Osteoarthritis of the joints is a chronic joint disease caused by metabolic disorders. As a result, there are degenerative, dystrophic changes and destruction of cartilage tissue.
It appears imperceptibly, but often develops very quickly. A person begins to feel pain in the joints when moving, there is stiffness and reduced mobility, especially in the mornings, while they are still "not in conflict". If discomfort occurs with uncomfortable movements or loads, and periodic pains appear, isit is very important to understand that these will not go away and without intervention the situation will only get worse.
Symptoms of osteoarthritis
Arthrosis of the large and medium joints seriously changes a person's lifestyle, worsening its quality and imposing restrictions. The development of the disease is like an avalanche and the treatment is usually associated with unbearable pain, which is a clear sign of wear and tear on the joints.
Symptoms of osteoarthritis of the joints depend on how badly the joint, cartilage and surrounding tissues are affected.
At the initial stage, arthrosis can be determined fairly accurately, treatment in this case is economical and does not require serious intervention and expensive drugs to treat arthrosis.
types of osteoarthritis
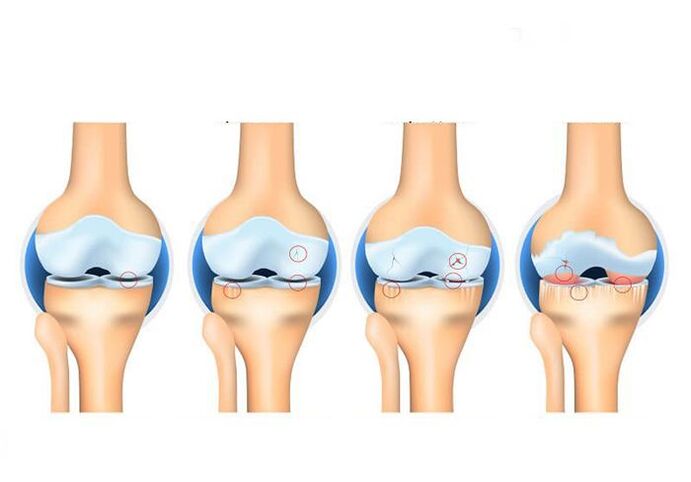
Osteoarthritis of the joints is classified according to several criteria. Depending on the degree of arthritic changes in the cartilage tissue, 4 stages of arthrosis are distinguished. Osteoarthritis is also divided into primary and secondary. The cause of the development of primary arthrosis are age-related changes. Secondary osteoarthritis occurs due to injuries and diseases of the joints (e. g. traumatic osteoarthritis or rheumatoid arthritis). The disease can also develop gradually over years or lead to the destruction of the joint after just a few years (progressive arthrosis).
There isTypes of osteoarthritis depending on the affected area:
- – arthrosis of the knee joint – arthrosis of the hip joint
- Uncovertebral arthrosis - arthrosis of the cervical vertebrae
- Vertebral arthrosis - damage to the spine
- Patellofemoral osteoarthritis is a form of gonarthrosis that affects the patella and part of the femur.
The degree of the disease is determined by the degree of damage to the cartilage tissue.
Arthrosis of the 1st degree - the cartilage tissue is slightly damaged, the person does not feel any discomfort;
Arthrosis II degree - osteophytes appear, the distance between the cartilages decreases, situational pains appear with clumsy movements;
Osteoarthritis III. Degrees - the cartilage tissue is destroyed in places and the bone tissue is exposed, the distance between the cartilages decreases, the pains are frequent and severe;
Arthrosis IV degree - a significant part of the cartilage tissue is destroyed by 60%, there is no gap between the bones, patients constantly experience severe pain, hyperthermia of the area above the joint occurs.
- A characteristic crunch during movements and a slight pain in the background;
- Limitation of joint mobility, discomfort with full physical activity;
- "Jumping" blood pressure indicators;
- headache and dizziness;
- convulsive syndrome and often muscle spasms;
- Visually observed deformity of the joint;
- swelling, hyperthermia, or redness of the area of skin over the diseased joint;
- Violation of motor function.
Why does the disease appear
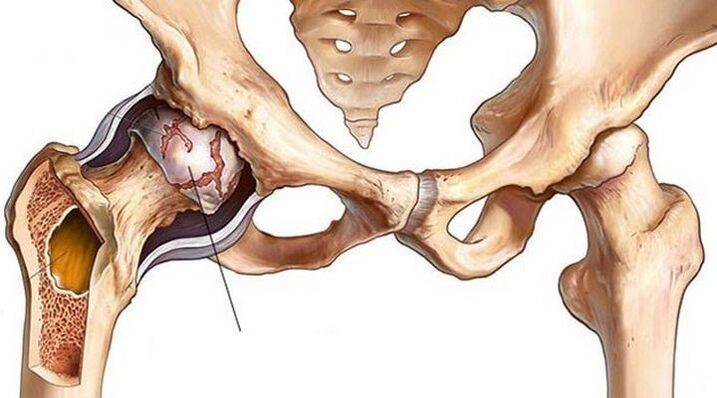
Arthrosis of the joints can manifest itself in any of the departments, but most often patients turn when arthrosis of the knee or hip joint makes itself felt. Shoulder arthrosis can be observed in the workplace if the hands are subjected to particular, specific strain.
The lesions differ in men and women.The strong half often suffers from osteoarthritis of the temporomandibular joint, wrist, ankle and lumbar spine. Women complain more about the chest and neck area, as well as the joints of the fingers and big toes.
The nature of the disease is determined by the location of the lesion. There are the following types:
- Arthrosis of the hip joint - coxarthrosis;
- Arthrosis of the knee joint - gonarthrosis;
- damage to the patella and part of the femur - patellofemoral arthrosis (a type of gonarthrosis);
- spinal disease - vertebral arthrosis;
- damage to the cervical spine - uncovertebral arthrosis.
The main reasons are:
- inflammatory process;
- professional sports;
- overweight;
- professional non-standard load, e. g. B. Squatting or kneeling;
- previous joint injuries (post-traumatic);
- hypothermia;
- heredity;
- age changes.
Osteoarthritis can occur as a disease in its own right or it can be the result of an ongoing disease, so it is important to know a person's history.
Diagnosing arthrosis of the joints
Osteoarthritis of the joints is detected by X-rays. The x-ray shows how the joint deforms and how much the joint space narrows. MRI or arthroscopy may also be necessary, but only in particularly complex and ambiguous cases. X-rays of the joints are usually sufficient to diagnose the disease.
To understand the presence of the disease, its severity and what disorders led to the disease, a comprehensive diagnosis is carried out.
First with the helpX-ray in different projectionsGet information about the degree of joint damage.
Tomography (magnetic resonance or computer) helpsRule out tumor processes.
Third, you needtake examsto understand whether osteoarthritis is an independent disease or a complication, as well as to determine the general condition of a person.
The complex of studies is the most informative and gives a clear idea of degenerative-dystrophic changes and helps to choose the optimal treatment plan.
treatment of osteoarthritis
As discussed above, osteoarthritis can develop due to many factors and the treatment plan is developed based on an understanding of the underlying causes and medications used to treat osteoarthritis are selected accordingly.
Treatment should be developed individually, based on the results of the diagnosis. Be sure to take into account the condition of the person, his existing diseases.

Restoration of the articular surface and cartilage tissue is not rapid. Effective drugs are prescribed that have side effects. And taking medication to achieve the desired result takes up to 6 months. Therefore, it is important to protect your health from side effects as much as possible.
Medical treatment of osteoarthritis
The main goal of such therapy is to eliminate the manifestations of arthrosis. Drug treatment of arthrosis of the joints includes:
- Non-steroidal anti-inflammatory drugs. With arthrosis, a person experiences pain, the joint becomes inflamed. To eliminate unpleasant symptoms and stop inflammation, this group of drugs is prescribed.
- Hormone injections in the joint. Corticosteroid medications are most commonly given in the acute stage of osteoarthritis.
- chondroprotectors. The main task of these drugs is to stop the degenerative processes in the cartilage tissue in order to prevent its further destruction.
- Intra-articular injections of hyaluronic acid. Hyaluronic acid preparations are similar to synovial fluid, which provides lubricity and smooth free movement in the joint. In osteoarthritis, the synovial fluid is not sufficiently secreted, so orthopedists often prescribe hyaluronic acid injections (injections into the joint in osteoarthritis).
- Biological therapy of arthrosis (PRP and cytokine therapy). A new innovative method of osteoarthritis therapy, which has recently been introduced into practice, but is gaining popularity. This is the use of drugs based on the patient's blood plasma enriched in platelets. Thanks to biological therapy, blood circulation in the joint is activated, the production of intra-articular fluid is activated and the cartilage tissue is supplied with nutrients.
Important!Drug treatment of osteoarthritis is effective in the early stages of the disease. Experts also emphasize that drug therapy cannot restore a damaged joint, but it allows eliminating symptoms and slowing the progression of arthrosis.
Physiotherapy and other conservative treatments for osteoarthritis
Physiotherapy is also used in the fight against osteoarthritis. Various procedures (laser, phonophoresis, electrophoresis, magnetotherapy, UVT) and exercise therapy are prescribed to improve metabolic processes, blood circulation and strengthen muscles.
In addition, with osteoarthritis, you just need to make a few lifestyle adjustments:
- Avoid Overloading - It's important to spread out the activity evenly and take breaks to avoid overloading the joint
- Watch the diet and monitor weight - since excess weight only aggravates the problem with the joints, you need to review your diet and reduce body weight
- Remember to be careful and avoid injury as much as possible
- Use additional support for movement - in the later stages of osteoarthritis, independent movement becomes questionable, requiring the use of a cane or crutches. For more comfortable walking, you can also use orthopedic insoles - they reduce the load on the joint.
There are also many folk recipes that "help to defeat arthrosis. "But even treating osteoarthritis at home does not always bring results. In addition, the use of all kinds of lotions and ointments of their own preparation most often only provokes allergic reactions and does not harm the health of the joint.
Surgical treatment of osteoarthritis

How to treat osteoarthritis if all the above methods do not work? In this case, surgical treatment of arthrosis is prescribed. Depending on the degree of damage to the joint, the individual characteristics of each patient, a type of operation is selected.
Joint arthroscopy is a non-traumatic procedure, an intra-articular intervention through multiple micropunctures in the joint. In arthrosis, it serves as a temporary measure for "joint cleaning": removal of cartilage parts, osteophyte proliferations that impair freedom of movement. Such treatment reduces pain in the joint, but it is not a solution to the problem of arthrosis.
Osteotomy is an operation to align the joint axis. The fact is that with arthrosis, as a rule, one part of the joint suffers more (it has a large load). The osteotomy redistributes the load on the joint. It should be noted that osteoarthritis is a progressive disease of the joints. Therefore, osteotomy is a way to delay further treatment, but not avoid it.
Joint arthroplasty is an effective and in some cases the only method of treating arthrosis of the joints. The essence of the operation is the removal of a joint destroyed by the disease and the implantation of an artificial endoprosthesis in its place. The artificial joint is selected individually, is ideally suited for each patient and, after a period of rehabilitation, fully restores the functions of the damaged joint.
Contraindications for arthrosis
What to look out for in osteoarthritis of the joints:
Shared Burdens- If you have osteoarthritis, you must refrain from lifting weights and excessive static loads. A walking stick can be used to relieve the joint. Shoes - Properly fitting shoes reduce stress on the joint. It is advisable to avoid high-heeled shoes.
The weight- Obesity is another factor in the progression of osteoarthritis. It is therefore important to maintain a healthy weight and eat a balanced diet.
Sportsmust also be checked. With arthrosis, it is necessary to exclude sharp jerky movements (contact sports, wrestling), long-distance running, lifting weights. However, this does not mean that physical activity should be stopped completely. Moderate activity only benefits the joint.
In addition to medical treatment, physiotherapy is actively used. These are magnetic therapy, electrotherapy, thermotherapy. In addition, physiotherapeutic exercises are recommended to strengthen the muscles around the affected joint and improve blood circulation.
A radical method of deforming arthrosis, which led to a deterioration in the quality of life, is often surgical intervention. In this case, either arthroscopy or arthroplasty is performed.
Arthroscopy is a procedure in which the worn top layer of the joint is removed and a partial prosthesis is put in its place. So you can eliminate pain and restore mobility.
Arthroplasty is the replacement of a joint with a prosthesis. It is appropriate in the case of severe destruction when the joint itself cannot reasonably be saved. The prosthesis has artificial cartilages that are anatomically identical to human ones.
Treatment of the disease in the initial stages is the provision of high-quality nutrition for cartilage tissues. For this purpose, the use of chondroprotectors, preferably flavonoids of natural origin, is recommended. Motor load is also necessary to improve blood supply to the bones and perichondrium.
Deforming osteoarthritis of the knee
Deforming arthrosis of the knee joint(gonarthrosis, DAK) is a chronic progressive disease of the articular cartilage. It is characterized by the destruction of articular structures, which is accompanied by pain, inflammation and a characteristic curvature of the limb ("legs with a wheel" or X-shaped deformation).
Causes of deforming osteoarthritis of the knee
Without adequate lubrication, the joint "dries out", cracks and loses height, exposing the heads of bones. In this case, the closing plate of the articular surface of the bone is left defenseless; Re-irritation of the numerous nerve endings located therein causes pain and discomfort.
The following factors or their combination can be the cause of a deforming arthrosis of the knee joint:
- the presence of diseases of the joints (and especially the knee) in relatives;
- genetic disorders associated with the formation of abnormal, unstable cartilage cells or their accelerated death;
- congenital and acquired malformations of the musculoskeletal system (flat feet, joint hypermobility, dysplasia, scoliosis, kyphosis and others);
- excessive stress from work, household or sport;
- Microtraumas and injuries of the knee joint and meniscus, operations on them, broken legs;
- Circulatory disorders (varicose veins, atherosclerosis, thrombosis and other vascular diseases), their consequences (preparatory osteochondritis), as well as other causes of persistent cramps in the legs;
- inflammatory diseases of the joints and tissues close to the joints (synovitis, bursitis, tendonitis, arthritis), including autoimmune nature (rheumatoid, psoriatic arthritis);
- Metabolic disorders (gout, diabetes mellitus);
- age-related aging processes of the joints and calcium leaching from the bones;
- hormonal disorders and changes in the hormonal background (for example, associated with estrogen deficiency in women);
- hypovitaminosis;
- overweight (observed in ⅔ of patients);
- physical inactivity.
But the main reason deforming osteoarthritis of the knee is so common is because of its structure. The knee joint has only one axis of movement (plane). Therefore, the range of permissible movements is very limited. A clumsy rotation can injure the tissue near the joint and trigger arthritic changes - after all, the painful knee is put under daily strain.
Deforming knee arthrosis can be caused by a variety of factors.

Symptoms of deforming arthrosis of the knee joint
Gradually increasing pain in the knee joint area. At first, the pain is felt only when moving - for example, when sharply stretching or bending the leg, there is a feeling of "unfortunately stepping on your foot. "In the early stages, pain may be episodic or so mild as to be uncomfortable. Then the pain intensifies after physical exertion or staying in the same position for a long time. The skin also becomes painful – it is sensitive to any touch, including clothing.
There are 3 types of specific pain in deforming arthrosis of the knee joint:
- Start (takes 15-30 minutes after the common exits from a long sleep);
- mechanical (noticeable during physical activity and disappears after rest);
- Blockage (sensation of a sharp pinching in the knee).
Symptoms of deforming arthrosis of the knee, as a rule, grow slowly, since the disease is not characterized by rapid progression. This is the insidious nature of arthrosis - gradually the patient gets used to the discomfort of the disease, the patient "gets used" to the pain, does not notice the deterioration and postpones the visit to the doctor.
Knowing the main symptoms of deforming knee arthrosis will help to identify the disease in time
Treatment of deforming arthrosis of the knee joint
The treatment of deforming arthrosis of the knee joint consists of the complex use of drugs, a dosed load on the joint, physiotherapeutic procedures and the use of orthopedic aids.
Alternating loading and unloading is extremely important during the course of treatment in order to avoid static loading of the knee. Orthopedic insoles, special shoes, canes, crutches, walking aids, ergonomic work and rest chairs also help to slow down the disease. Orthoses with variable stiffening are particularly effective, as they make it possible to model the physiological leg axis and compensate for the deformity.
In the early stages of deforming arthrosis of the knee joint, the aim of treatment is to restore the destroyed joint and ligament apparatus, to relieve pain and increase the range of motion. Later - in relieving the patient's condition. For this, remedial arthroscopy (washing with antiseptics) is performed if a piece of osteophyte is broken off, corrective osteotomy (correction of a curved bone), endoprosthetics (replacement) of the joint.
In addition to orthopaedists, physiotherapists and chiropractors, specialists in movement therapy and therapeutic massage and surgeons provide information on the treatment of deforming arthrosis of the knee joint.
Treatment of deforming arthrosis of the joints is a complex and lengthy process that requires a holistic approach.

physical therapy
Among other physiotherapeutic methods of treating deforming arthrosis of the knee joint are used:
- laser and magnetic therapy;
- microwave therapy;
- shock wave therapy;
- amplipulse;
- ultrasound therapy;
- electrophoresis with analgin, novocaine, chymotrypsin, etc. ;
- phonophoresis with glucocorticoids;
- paraffin and ozokerite applications;
- cryotherapy;
- Acupuncture;
- joint traction and exercise therapy;
- balneotherapy.
Massage for deforming arthrosis of the knee joint
Therapeutic and lymphatic drainage massage for deforming arthrosis of the knee joint, as well as manual therapy are performed by a specialist after relieving inflammation in the joint. For self-massage at home, stroking and rubbing are recommended, as well as movements aimed at stretching muscles and ligaments, a deep warm-up (done last, after a warming effect). Self-massage goes well with local irritants and essential oils. Remember that with deforming arthrosis of the knee joint, both joints are massaged, even if only one is affected.
Exercises for deforming arthrosis of the knee joints
Remedial gymnastics (exercise therapy) for deforming arthrosis of the knee joint is carried out sitting or lying down, water gymnastics is also effective. An individual set of exercises for deforming arthrosis of the knee joint is put together by an instructor. Below we offer a short warm-up aimed at strengthening the leg muscles.
- Sit on the floor, legs straight, emphasis on hands behind back. Bend and flex your toes.
- The starting position is the same, slowly bend your leg, at the end of the movement put your toe on the floor. Repeat with foot behind other foot.
- Continuing in the same starting position, raise the extended leg in front of you, toe towards you.
- Without changing the starting position, we draw our hands to the toes of the straightened legs.
- Sit on the floor, hug your bent knee and try to lift your other leg off the floor.
- Sit on the floor and spread your legs shoulder-width apart. Twist your legs one at a time so that the toe moves 180 degrees.
- Sitting on the floor, legs bent. Roll your foot from heel to toe and feel the work in the back of your thighs.
Excellent! Do exercises to deform arthrosis of the knee joint at least 3-6 times a day.
Medication for deforming arthrosis of the knee
Drug treatment of deforming arthrosis of the knee joint allows you to quickly stop acute pain, reduce inflammation and swelling, improve joint nutrition. Therefore, drugs are used at all stages of the disease and help restore knee mobility.
chondroprotectors
Chondroprotectors in the form of tablets, capsules, sachets and injections are used to regenerate and preserve synovial cartilage.
antiphlogistic
Steroids and nonsteroidal anti-inflammatory drugs are used to treat deforming arthrosis of the knee joint. They are prescribed in the form of tablets, injections, sachets, creams, ointments and other products for external and internal use.
Anti-inflammatory drugs can be used in conjunction with anesthetics that are injected into the joint cavity to create a blockage.
antispasmodics
Removal of spasms is necessary to return the patient to normal activities and normal tissue nourishment.
angioprotectors
With deforming arthrosis of the knee joint, preparations based on horse chestnut and others are used.
heating means
Among the warming means, it is worth highlighting preparations based on natural ingredients: snake and bee venom, paprika, mustard.
All of these drugs improve blood supply to tissues and distract from pain.
Nutrition in deforming arthrosis of the knee
A healthy diet for deforming arthrosis of the knee joint includes dishes with a reduced content of trans fats and "fast" carbohydrates. Preference is given to lean meat and fish, seafood and vegetables, steamed, stewed in foil or under a lid. Fruits, berries are also usefuland drinks rich in antioxidants - wild plants, blueberries, cranberries, lingonberries, high-quality green tea and coffee. You can also eat whole grain cereals, legumes.
But potatoes, white bread, sweets, ready meals, fast food and alcohol should be excluded.
If you are overweight and have deforming knee osteoarthritis, consider low-carb diet options.



























